© Copyright 2007 Health Grades, Inc. All rights reserved.
Hospital Report CardsTM Methodology 38
May not be reprinted or reproduced without permission from Health Grades, Inc.
Appendix D
Methodology Enhancements for 2007 Ratings Models
The following changes were determined and implemented after input from outside coding and clinical
experts. For the following service lines, we describe the changes for each rated cohort and provide the
rationale behind these changes.
·
All Service Lines
·
Cardiac
·
Orthopedic
·
Vascular
All Service Lines
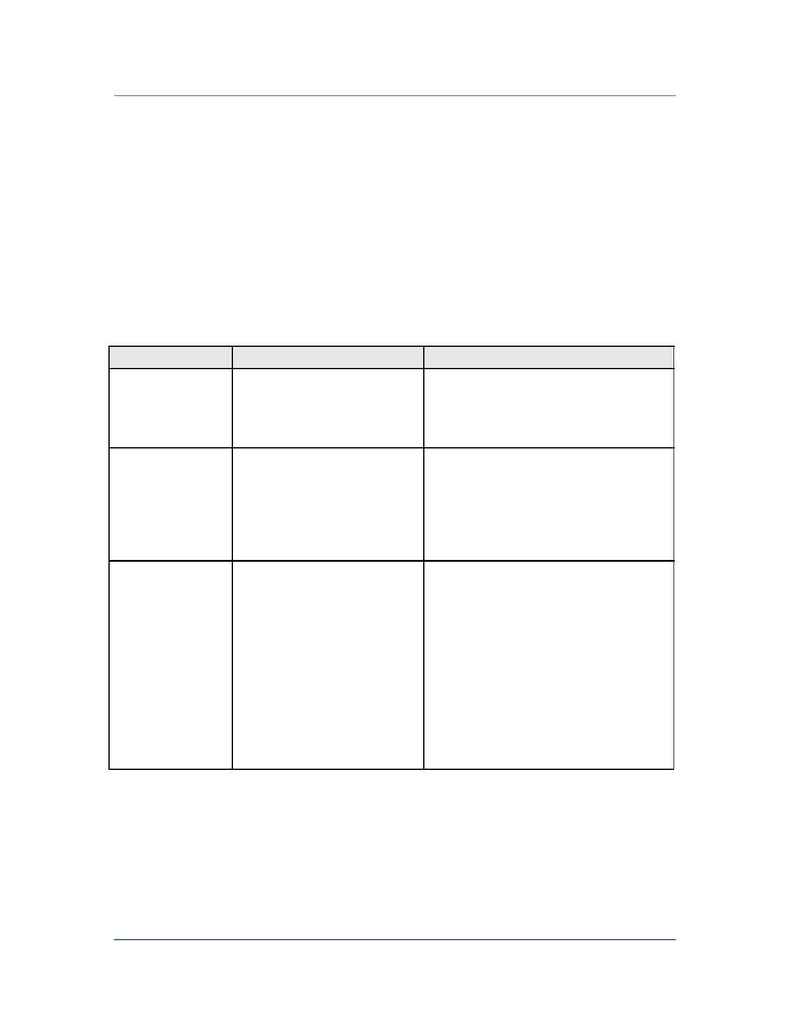
Cohorts Affected
2007 Ratings' Model Change
Rationale for Changes
All
Decreased national volume for
potential risk factors from 1% to 0.5%
Some risk factors, while infrequent, are highly
correlated with the outcome of measure and thus
should be risk adjusted for the patient population
evaluated.
All
Required a hospital to have a total of
30 cases over the three year period
and a minimum of five cases in the
most current year of analysis (2005)
to be rated in a cohort.
Previously hospitals were required to have a
minimum of 30 cases over the three year period
and one case in the most current year of analysis.
Increasing the cases in the most current year of
analysis ensures hospitals appropriately included
in the cohort.
All diagnosis cohorts:
Heart Attack, Heart
Failure, Atrial
Fibrilation, Community
Acquired Pneumonia,
COPD, Stroke, Bowel
Obstruction, GI Bleed,
Pancreatitis,
Pulmonary Embolism,
Sepsis, Diabetic
Ketoacidosis
Excluded patients with any code for
secondary cancer diagnoses
(196.0-196.9, 197.1-197.8,
198.0-198.8, 198.81-198.82, 198.89)
Patients with metastasized cancers present at
various stages of illness with different end-of-life
directives. Because these directives cannot be
identified in administrative data, these patients
were excluded from analysis.
