SSMC Employee Health Benefit Plan
80
·
The health care professional engaged for purposes of a consultation shall be an individual
who is neither an individual who was consulted in connection with the Adverse Benefit
Determination that is the subject of the appeal, nor the subordinate of any such in dividual;
and
·
In the case of a Claim Involving Urgent Care, provide for an expedited review process
pursuant to which a request for an expedited appeal of an Adverse Benefit Determination
may be submitted orally or in writing by the Claimant; and all necessary information,
including the Plan's benefit determination on review, shall be transmitted between the Plan
and the Claimant by telephone, facsimile, or other available similarly expeditious method.
e. Timelines for Plan Notification of Appeal Determinations. The Plan must send written or electronic
Notification for Adverse Benefit Determinations. See Manner and Content of Notification described
later.
1) Calculating Time Periods for Plan Notice of Determination Upon Review (Appeals Review).
Time periods start at the time the appeal is filed in accordance with reasonable requirements of the
Plan without regard to whether all necessary information accompanies the filing.
When period is extended due to Claimant's failure to provide necessary information, the period is
tolled (not counted) from the date Notification of extension is sent to the Claimant until the date
the client responds to request for additional information. Then countdown continues. Days and
hours are counted on calendar day bas is rather than business day basis.
2) Timelines for Plan Notification. Claimants shall be notified of the Plan's benefit determination
upon review as soon as reasonably possible considering medical circumstances but not later than
the following timelines:
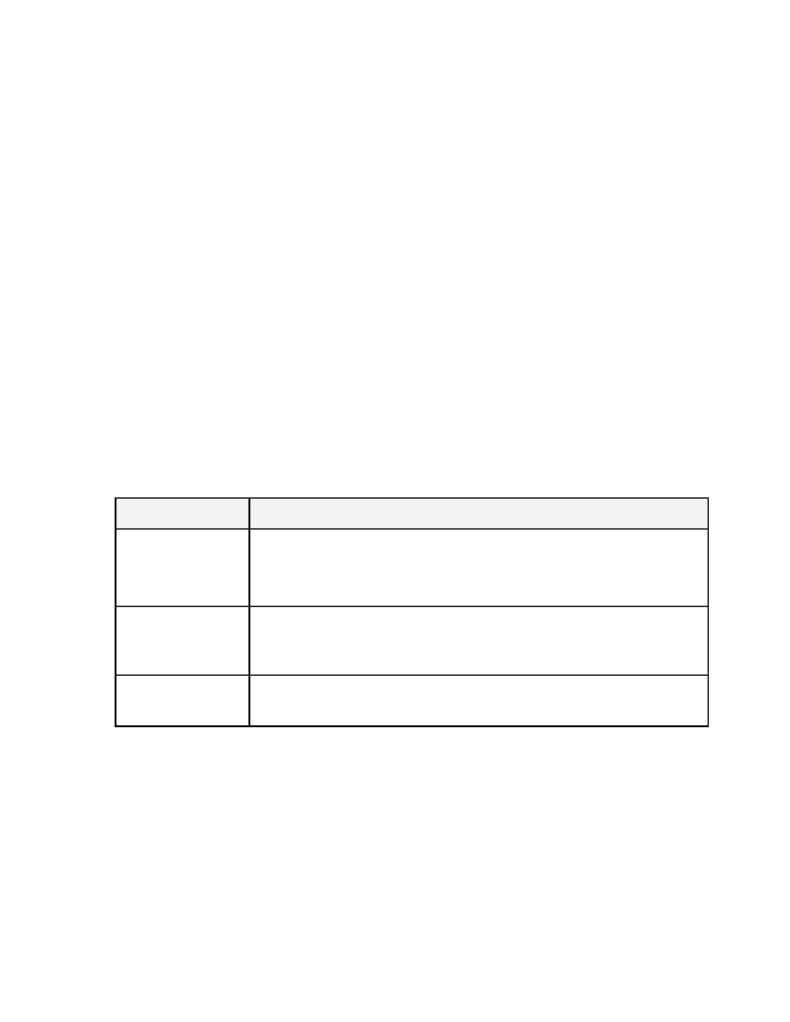
Type Claim
Timeline for Plan Notice of Benefit Determination Upon Review
Urgent Care
(Includes Concurrent
Care involving Urgent
Care)
Within 72 Hours after Claimants appeal of Adverse Benefit Determination for Plan
Notice upon review, whether Adverse Benefit Determination or not.
Pre-Service
(Claims involving Non-
Urgent Care)
Within 30 calendar days after Claimants appeal of Adverse Benefit Determination for
Plan Notice upon review, whether Adverse Benefit Determination or not.
Post-Service
Within 60 calendar days after Claimants appeal of Adverse Benefit Determination for
Plan Notice upon review, whether Adverse Benefit Determination or not.
f. Manner and Content of Notification of Benefit Determination upon Plan Review. The Claimant
will be provided with written or electronic Notification of any Adverse Benefit Determination. Any
electronic Notice must comply with the standards imposed by federal regulations concerning electronic
Notifications.
·
The specific reason or reasons for the adverse determination;
·
Reference to the specific Plan provisions on which the benefit determination is based;
·
A statement that the Claimant is entitled to receive, upon request and free of charge, reasonable
access to, and copies of, all documents, records, and other information Relevant to the Claimant's
Claim for Benefits.
