SSMC Employee Health Benefit Plan
78
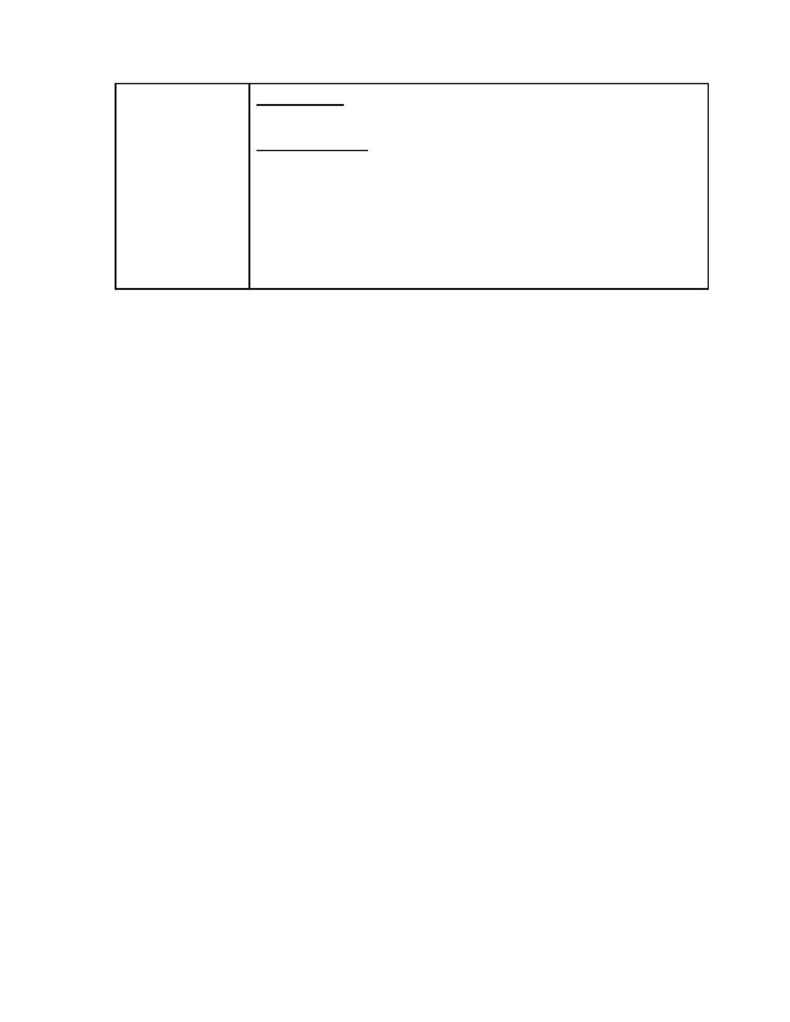
Post-Service
"Clean Claims"
Within 30 calendar days for Plan Notice of Adverse Benefit Determination.
One Time Extension
·
Up to 15-calendar days extension due to matters beyond control of Plan
Administrator (or Claims Administrator acting for the Plan Administrator).
·
Notice of such delay will be sent to the Claimant before the end of the initial 30-day
period and will include the circumstances that required the extension.
If extension is due to failure of the Claimant to submit necessary information, then
Notice of extension shall specifically describe required info and the Claimant shall be
given at least 45 days from receipt of the Notice to provide the information.
e. Manner and Content of Plan Notification. According to the federal regulations, a Claimant must be
provided with written or electronic Notification of any Adverse Benefit Determination. Any electronic
Notification must comply with the standards imposed by federal regulations concerning electronic
Notifications. The Plan may provide its written notice on the Explanation of Benefits or as a separate
written notice.
Note: In the case of an Adverse Benefit Determination by the Plan concerning a Claim involving Urgent Care,
the information described below may be given to the Claimant orally provided that a written or electronic
Notification is furnished to the Claimant not later than 3 days after the oral Notification.
1) Notice Contents. Plan Notifications will be written in a manner designed to be understood by the
Claimant and will include:
·
The specific reason or reasons for the adverse determination;
·
Reference to the specific Plan provisions on which the determination is based;
·
A description of any additional material or information necessary for the Claimant to perfect
the Claim and an explanation of why such material or information is necessary;
·
A description of the Plan's review procedures and the time limits applicable to such
procedures, including a statement of the Claimant's right to bring a civil action under section
502(a) of the ERISA Retirement Income Security Act following an Adverse Benefit
Determination on review. (Section 502 (a) of the Act provides that Participants and
beneficiaries may bring a civil action to clarify their rights to benefits);
·
If an internal rule, guideline, protocol, or other similar criterion was relied upon in making the
adverse determination, either the specific rule, guideline, protocol, or other similar criterion; or
a statement that such rule, guideline, protocol, or other similar criterion was relied upon in
making the adverse determination and that a copy of such rule, guideline, protocol, or other
criterion will be provided free of charge to the Claimant upon request;
·
If the Adverse Benefit Determination is based on a Medical Necessity or Experimental
treatment or similar exclusion or limit, either an explanation of the scientific or clinical
judgment for the
determination, applying the terms of the Plan to the Claimant's medical
circumstances, or a statement that such explanation will be provided free of charge upon
request.
·
In the case of an Adverse Benefit Determination by the Plan concerning a Claim Involving
Urgent Care, a description of the expedited review process applicable to such Claims.
