SSMC Employee Health Benefit Plan
77
necessary information accompanies the filing. When period is extended due to Claimant's failure
to provide necessary information, the period is tolled (not counted) from the date the Notification
of extension is sent to the Claimant until the date the client responds to request for additional
information. Then countdown continues. Days and hours are counted on calendar day basis rather
than business day basis.
2) Timelines Based on Type Claim. The timelines for the Plan Notice of benefit determination
varies based on whether Claim is considered an Urgent Care Claim; Pre-service Claim or Post-
Service Claim. The Plan Notification will be sent to the Claimant as soon as possible after receipt
of a Claim, taking into account medical circumstances, but not later than timelines shown below:
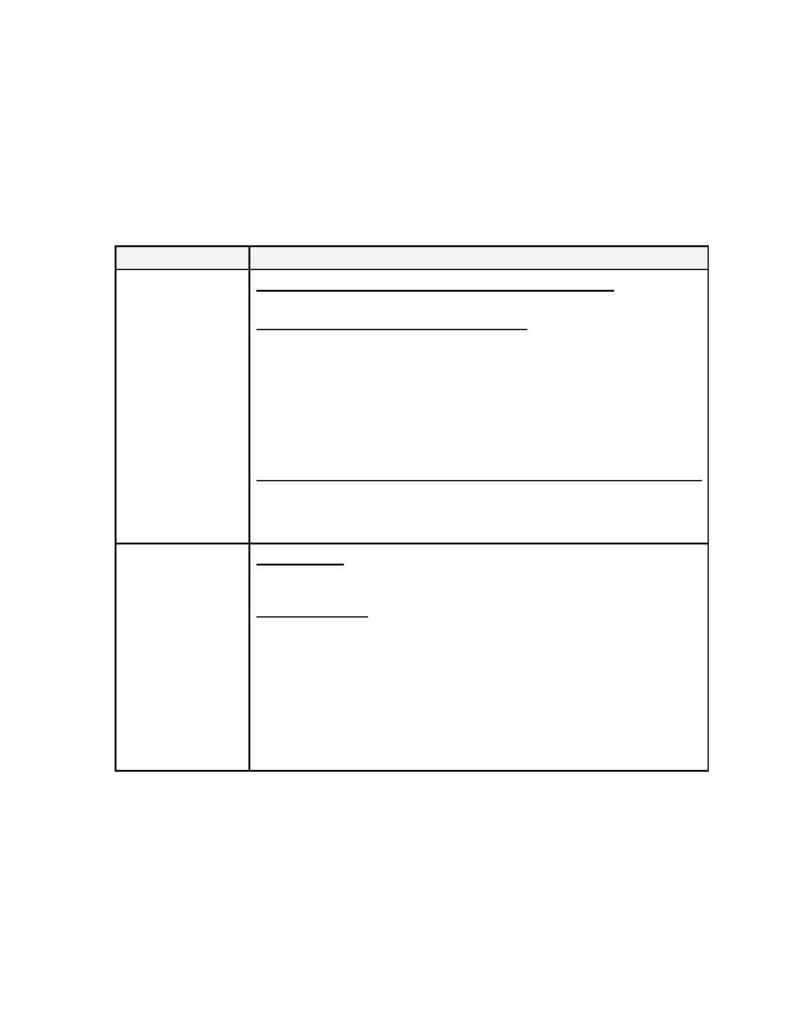
Type Claim
Timeline for Notice of Initial Benefit Determination
Urgent Care
"Clean Claims" (does not require additional info from Claimant)
·
Within 72 Hours for Plan Notice whether Adverse Benefit Determination or not.
Claimant Fails to Provide Necessary Information.
·
Within 24 Hours for Plan Notice of Claimant's failure to provide necessary
information. (Claimant will be given reasonable time to respond, but not less than
48 hours to provide specified information).
·
Within 48 hours for Plan Notice, whether Adverse Benefit Determination or not,
after the earlier of:
The Plan's receipt of the specified information, or
The end of the period given for providing information.
Concurrent Claims Request to Extend Course of Treatment Involving Urgent Care
·
Within 24 Hours for Plan Notice whether Adverse Benefit Determination or not
(when request is made for care at least 24 hours prior to expiration of the current
prescribed period of time or number of treatments).
Pre-Service
(Claims involving
Non-Urgent Care)
"Clean Claims"
Within 15 calendar days for Plan Notice whether Adverse Benefit Determination or
not.
One Time Extension
·
Up to 15-calendar days extension due to matters beyond control of Plan
Administrator (or Claims Administrator acting for the Plan Administrator).
·
Notice of such delay will be sent to Claimant before the end of the initial 15-day
period. Notice will include circumstances requiring extension and the date by which
the Plan expects to render a decision.
If extension is due to failure of the Claimant to submit necessary information, then
Notice of extension shall specifically describe required info and the Claimant shall be
given at least 45 days from receipt of the Notice to provide the information.
