SSMC Employee Health Benefit Plan
26
2. Notification of Qualifying Events. You, as an Employee of
SSMC
, or your Dependents are responsible
for notifying the SSMC Human Resources Department in writing within 60 days following the date of a
divorce, legal separation, Social Security disability, child losing eligibility status, or other qualifying event
that would otherwise cause Plan coverage for you or your Dependent(s) to end. The SSMC Human
Resources Department will send written notice of your COBRA rights, your costs, and election forms for
COBRA enrollment within 14 days after your notification to the SSMC Human Resources Department.
In case of resignation or termination of employment (other than for gross misconduct), reduction of work
hours, or the death of an Employee, the SSMC Human Resources Department will notify the qualified
beneficiaries of their option to continue their current coverage within 14 days.
Please Note
If the SSMC Human Resources Department does not receive written notice of a qualifying event within 60 days after
such event, COBRA continuation will not be available and Plan coverage will stop on the date eligibility ended.
SSMC administers COBRA enrollment and billing procedures.
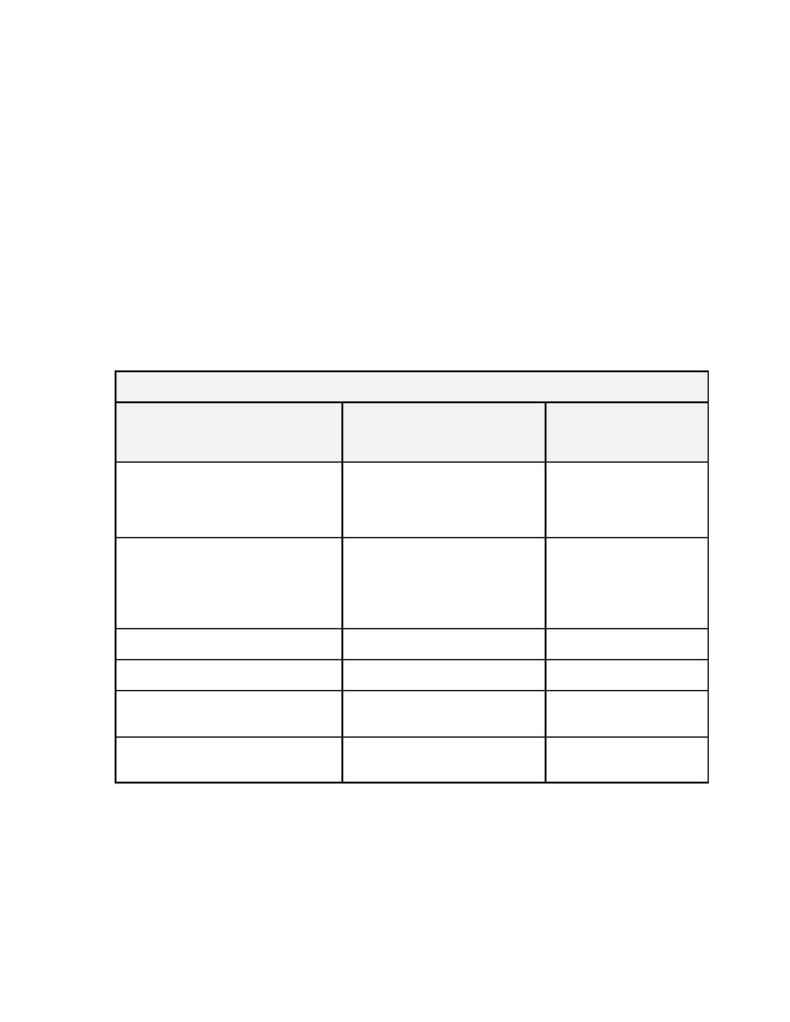
3. COBRA Continuation Periods. The following chart outlines the qualifying event and the maximum
length of COBRA continuation available for each event:
In no event, will COBRA continuation exceed more than 36 months for any beneficiary
When continued coverage maybe
elected? ("Qualifying Events")
Who may elect continued
coverage?("Qualified
Beneficiaries")
For how long may coverage
be continued?
Termination of employment or loss of
hours for Employee (other than for gross
misconduct), or reduction in hours of
Employee
Employee, Spouse and Dependent
children
18 months
Termination of employment or
reduction of hours of Emp loyee. (other
than for gross misconduct) when
Employee or Dependent is eligible for
Social Security Disability
Employee, Spouse and Dependent
children
29 months
(Includes the additional 11
months due to Social
Security disability)
Death of Employee
Spouse and Dependent children
36 months
Divorce or legal separation
Spouse and Dependent children
36 months
Employee becomes entitled for
Medicare
Spouse and Dependent children
36 months
Dependent child becomes ineligible
pursuant to Plan
Dependent child
36 months
Qualified Beneficiaries who receive Social Security disability benefits could be eligible for an additional 11
months extending the 18-month continuation period to 29 months. To be eligible for this extension, the
beneficiary must have been disabled at the time coverage ended or become disabled within 60 days after
the start of his or her COBRA continuation period. A copy of the Social Security determination showing
the date of disability must be sent to the SSMC Human Resources Department within 60 days following the
date Social Security approved the disability and within the first 18 months of COBRA continuation. This
extension applies to the disabled beneficiary (Employee, Spouse or child) and family members enrolled in
family coverage, if applicable.
