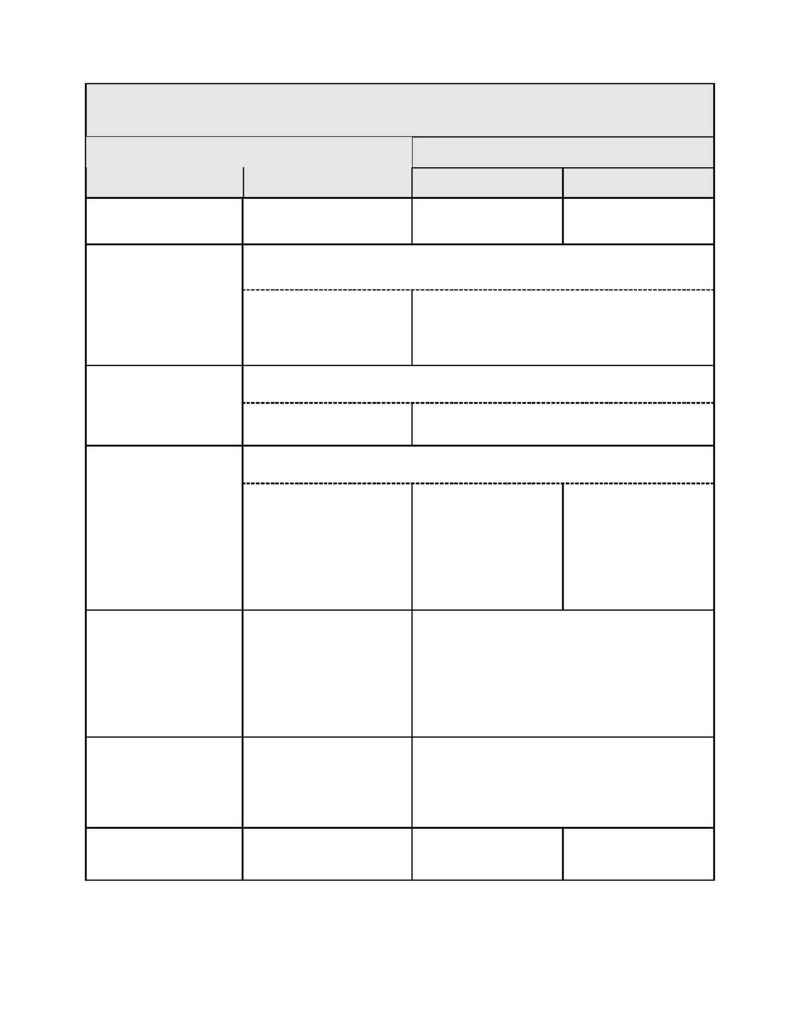
SSMC Employee Health Benefit Plan
13
Remember: Benefits could be reduced if you or your Dependent fails to follow the mandatory phone call procedures for
most Inpatient admissions or before home care starts. See Section III Benefits Management Program for details.
All payments are based on Allowable Fees.
Out-of-Network Providers
Schedule A MEB
Covered Services
SSMC / PHO Area
Network Providers
Living in PHO Area
Living 0utside PHO
Area
Speech Therapy
$5.00 Network Copayment
per visit.
After Deductible, Plan
pays 70%
After Deductible, Plan
pays 80%
Coverage is limited to 15 visits when rendered within six months after the date of the
family member death. Includes services by pastoral counselor.
Bereavement Counseling
After $5.00 Copayment per
visit, then Plan pays 50%
Provider may balance bill up
to Network Allowance.
After Deductible, Plan pays 50%. Balance does not
count toward Out-of- pocket limits. Provider balance
bills up to their charges.
Coverage is limited to one wig and up to maximum benefit of $500 per Lifetime when
wig ordered by Physician for hair loss due to radiation therapy or chemotherapy.
Hairpieces/Wigs
Plan pays 100% up to
maximum benefit.
No Deductible. Plan pays 100% up to maximum benefit.
Limited to 12 visits per Calendar Year for any combination of Network and Out-of-
Network Providers.
Acupuncture
SSMC: Full Benefits when
part of the SSMC pilot
program. Does not apply to 12
visit limit.
Area PHO Provider: $5.00
Network Copayment per visit
when rendered by PHO
Certified Acupuncturist.
After Deductible, Plan
pays 70%
(Must be rendered by
Certified Acupuncturist.
and ordered by attending
Medical Doctor)
After Deductible, Plan
pays 80%
(Must be rendered by
Certified Acupuncturist.
and ordered by attending
Medical Doctor)
Sleep Apnea Studies
SSMC ONLY (When part of
the SSMC pilot program).
Inpatient: After Inpatient
Deductible, Plan pays 100%.
Outpatient: $5.00 Copayment
per visit.
Area PHO Provider: Not
Covered
Not Covered
Weight Reduction
SSMC ONLY (When part of
the SSMC pilot program).
$5.00 Copayment per visit.
Area PHO Provider: Not
Covered
Not Covered
DME, Prosthetics, Other
Covered Services Not
Listed Above
Plan pays 100%
After Deductible, Plan
pays 70%
After Deductible, Plan
pays 80%
