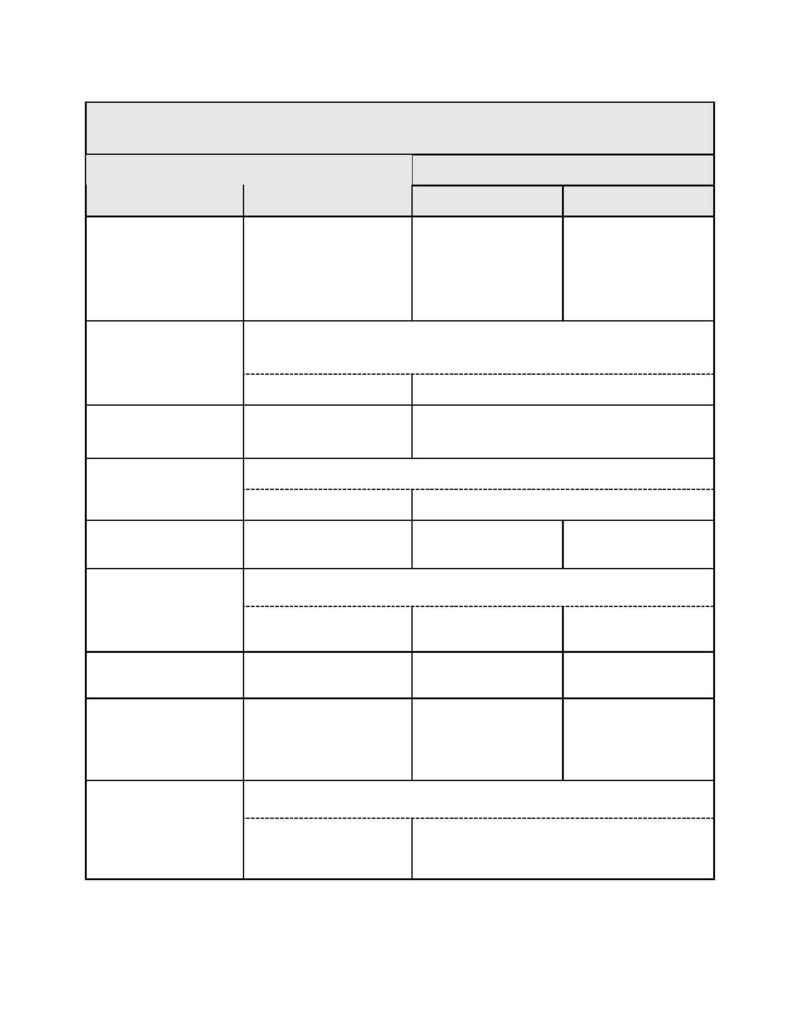
SSMC Employee Health Benefit Plan
11
Remember: Benefits could be reduced if you or your Dependent fails to follow the mandatory phone call procedures for
most Inpatient admissions or before home care starts. See Section III Benefits Management Program for details.
All payments are based on Allowable Fees.
Out-of-Network Providers
Schedule A MEB
Covered Services
SSMC / PHO Area
Network Providers
Living in PHO Area
Living 0utside PHO
Area
Ambulance
Emergency and Non-
Emergency: Plan pays 100%
Emergency:
No Deductible. Plan pays
100%
Non-emergency: After
Deductible, Plan pays
80%
Emergency:
No Deductible. Plan pays
100%
Non-emergency: After
Deductible, Plan pays 70%
Medical Emergency Care is initial care rendered within 12 hours after onset of sudden
and serious Illness or treatment of Injury started within 72 hours of an accident and
Incurred within 90 days following the accident.
Medical Emergency Care
Plan pays 100%
No Deductible. Plan pays 100%
Diagnostic Tests (X-rays,
labs, machine tests and
interpretations)
Plan pays 100%
No Deductible. Plan pays 100%
Covered when rendered within seven days before scheduled Hospital admission.
Pre-Admission Testing
Plan pays 100%
No Deductible. Plan pays 100%
Surgery
Plan pays 100%
After Deductible, Plan
pays 70%
After Deductible, Plan
pays 80%
Coverage includes acupuncture instead of general anesthesia during covered surgical
procedures.
Anesthesia
Administration
Plan pays 100%
After Deductible, Plan
pays 70%
After Deductible, Plan pays
80%
Second Surgical Opinion
$5.00 Network Copayment
per visit.
After Deductible, Plan
pays 70%
After Deductible, Plan pays
80%
Physician Inpatient Visits
Medical/Surgical
$5.00 Network Copayment
per visit
After Deductible, Plan
pays 70%
Plan pays 100% of
Allowable Fees for the
first 120 days, then after
Deductible, Plan pays
80%
Coverage is limited to one visit per day for which room and board benefits are
available up to 90 benefit days per each Covered Person's Lifetime.
Mental Illness
$5.00 Network Copayment
per visit
After Deductible, Plan pays 50% of Allowable Fees up
to coverage limits (Out-of-Pocket maximum does not
apply)
