SSMC Employee Health Benefit Plan
6
Federal Newborn/Maternity Provision/ERISA Notice. This notice is mandated by federal ERISA
requirements. According to the Newborns' & Mothers' Health Protection Act, a federal law, a health plan,
or its managed care program, that offers coverage for Hospital stays in connection with childbirth cannot
limit that coverage to less than a 48-hour Hospital stay following an uncomplicated normal delivery; or less
than a 96-hour Hospital stay following a cesarean section delivery. In addition, the health plan cannot
restrict benefits for any portion of the required minimum stays in a way that is less favorable than the
benefits provided for any preceding portion of the stay.
7. Federal Mastectomy Provision/ERISA Notice. This notice is mandated by federal ERISA requirements.
On October 21, 1998, the federal government amended ERISA to add a new section that requires group
health plans providing medical and surgical benefits with respect to a mastectomy to provide the following
coverage to a plan participant who elects breast reconstruction in connection with the mastectomy:
a. Reconstruction of the breast on which the covered mastectomy has been performed.
b. Surgery or reconstruction of the other breast to produce symmetrical appearance; and
c. Coverage for prostheses and physical complications of all stages of a covered mastectomy, including
lymphedema;
d. Coverage to be provided in a manner determined in consultation with the attending Physician and the
patient.
8. Benefit Schedule A. Out of PHO Network Benefits may differ for Covered Persons living inside or
outside the PHO area. These differences will be noted
.
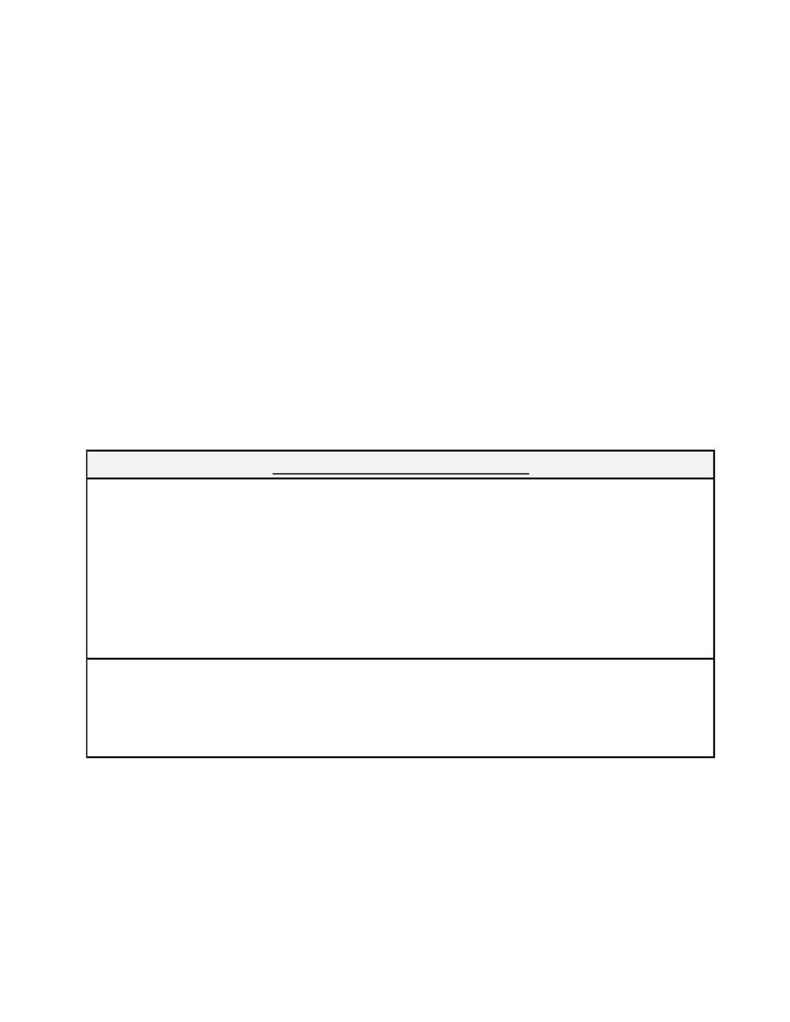
Schedule A Deductibles and Copayments
Unless shown otherwise, the Plan Deductibles and Percentage Copayments apply to Providers out of the PHO
area Network. The Inpatient Deductible applies to the PHO Area Network Hospitals or Substance Abuse
Facilities. The Network Copayments apply only when shown for covered PHO Network expenses.
Annual Deductible: The part of the Allowable Fees that the participant must pay each Calendar Year.
Benefits are based on the balance.
Percentage Copayment: The portion of Allowable Fees paid by the Pla n (usually after Deductible is taken).
Network Copayment: The portion of the Network allowable fee paid by the participant. This Copayment does
not count toward Hospital and Medical Expense Deductible or Out-of-Pocket Maximums.
Some specialized Covered Services and procedures are not available from PHO Providers. If you or
your Dependents require such services, coverage will be provided at PHO Network levels. Before
seeking this treatment, be sure to confirm with the Claims Administrator that the service or procedure is
not available in the PHO Network. The Claims Administrator's phone number is listed in the
Introduction section and on your Plan identification card.
