Unit-Specific Pharmacists
Vol. 28 No. 1 · January 2003 ·
P&T
®
57
by virtue of their positive interpretation. Our presence on the
patient-care units has added a degree of security that may not
be easy to quantify, although it has been felt and greatly ap-
preciated. Our attitudes, as well as our responsibilities and ac-
countability, have changed. As time passes and growth con-
tinues, methods of data collection may be altered to absorb new
clinical plans.
We are now researching the development of a patient-safety
program devoted to cardiac anomalies to screen patients who
are taking drugs that interact with the specific cardiac indica-
tors. As we peruse the available literature, we expect to uncover
new areas that need to be addressed, thereby expanding our
services to patients and to specialties within allied health care.
The unit-specific pharmacist program, originally designed
to prevent medication errors prospectively, has had a benefi-
cial effect on the hospital's other departments and services. The
program has defined and improved our role with respect to the
nutrition-support team and to the pharmacists who accom-
pany the clinical dietitians on daily rounds as they diligently
evaluate each patient and custom-tailor their respective nutri-
tion formulas. The clinical dietitians and the pharmacists have
worked together to create an interdisciplinary "performance
improvement key process" for the past year, which has been
very educational.
We have discovered that many of our allied health staff
members are flourishing because of the improved communi-
cation from the pharmacy. In response to this benefit and
as an extension of the program, we have created "Newslet-
ter Live," an educational, quarterly seminar presented by
the director of pharmacy. Since its inception, the seminar,
which is open to all hospital staff members, has become a
well-attended and a highly anticipated event. Sessions feature
current medication information, pharmacy policy updates,
and relevant facts, extracted from our pharmaceutical journal
readings that we have compiled into an easy-to-follow outline.
This program has greatly improved communication channels
within the multidisciplinary team and has allowed a forum for
the exchange of ideas between professionals.
It was also a challenge for us to convince the pharmacy staff
of the benefits of the new program. Some pharmacists who
had originally been skeptical about the sudden role change
needed reassurance that their expertise would be necessary
on both sides of the program. With time, some staff members
became interested in participating in the program as they
grew comfortable in becoming more visible within the hos-
pital. We needed to ensure that the functions of the pharma-
cists who remained in the pharmacy complemented, but did
not impede, the development of the new system. We consid-
ered it essential that each person be incorporated into the new
plan and not be ignored or forced into a role that would fos-
ter resentment or insecurity.
SUMMARY
Our goal with the unit-specific pharmacist program was
to address the need to prevent medication errors and to use
the pharmacist's knowledge and expertise, virtually at the
patient's bedside. The benefits of the program were far
greater than we anticipated. A major benefit was an in-
creased awareness that flexibility can be incorporated into
any hospital structure by using resources that are already
in place within the multidisciplinary team.
SUGGESTED READINGS
Crane V. Critical success factors in preparing for a JCAHO survey.
Pharmacy Practice News,
February 1722, 2002.
Guharoy R. Pharmacy paradigm shift: The challenges in the new mil-
lennium. The Pharmacist May/June 69, 2001.
Johnson N. Assessing the impact of outcomes projects: Take your lead
from the AHRQ approach. Formulary 2002;37:148158.
Johnson S, Blanchard K. Who Moved My Cheese? New York: Putnam;
1998.
Joint Commission on Accreditation of Healthcare Organizations. Com-
prehensive Accreditation Manual for Hospitals: The Official Hand-
book (CAMH).
Oakbrook Terrace, IL: 2000.
Massaro FJ. Improving a medication error monitoring program at an
acute-care hospital. Hosp Pharm 2002;37(3):259266.
McDaniel MR, DeJong DJ. Justifying pharmacy staffing by presenting
pharmacists as investments through return-on-investment anal-
ysis. Am J Health Syst Pharm 1999;56:22302234.
McWhinney BD. Reducing the Human and Economic Costs of Drug
Therapy Complications: Responding to the Medication Safety Issue
.
Dublin, OH: Cardinal Health, Inc; 1998.
Schneider PJ. Five worthy aims for pharmacy's clinical leadership to
pursue in improving medication use. Am J Health Syst Pharm
1999;56:25492552.
Weidle P, Bradley L, Gallina J, et al. Pharmaceutical care intervention
documentation program and related cost savings at a university
hospital. Hosp Pharm 1999;34(1):4352.
Zachry WM, Bootman JL. The role of the pharmacist in reducing pre-
ventable adverse drug events. P&T 2001;26(8):436440.
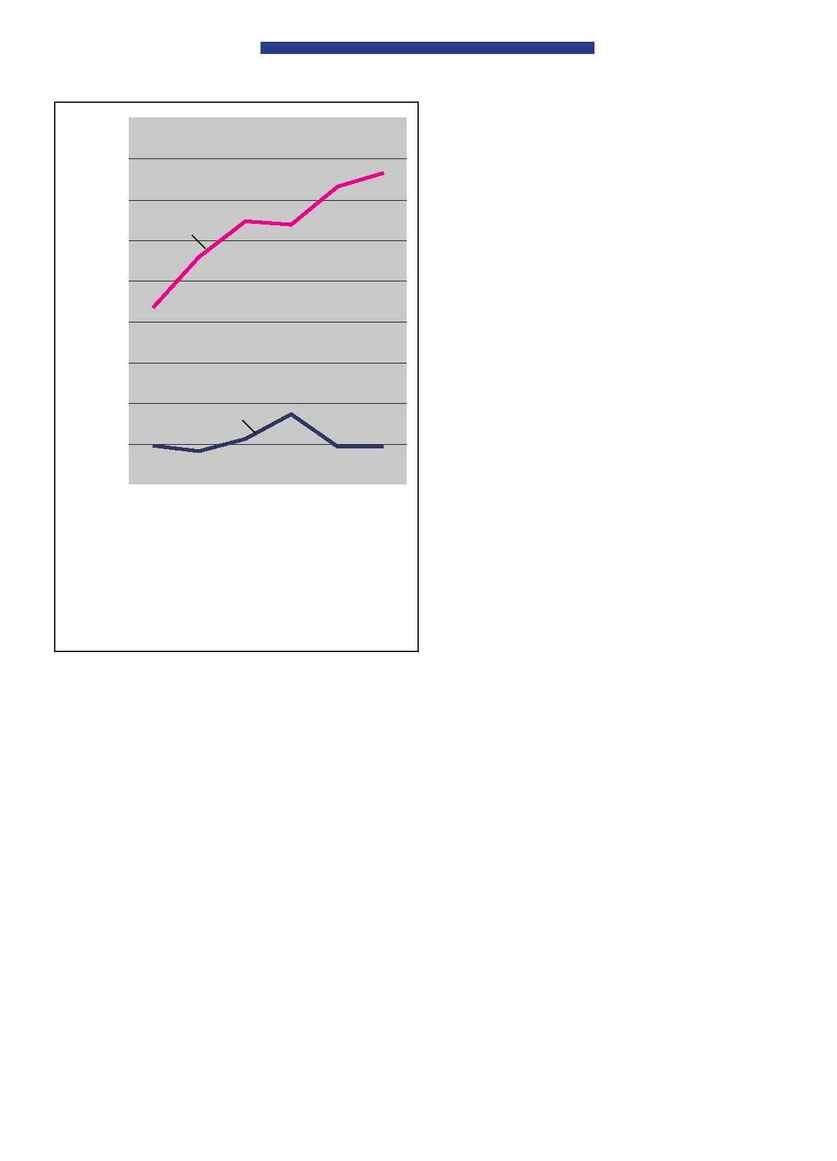
450
400
350
300
250
200
150
100
50
0
Sept.
Oct.
Nov.
Dec.
Jan.
Feb.
Number of
48
41
56
87
47
47
interventions
20002001
Number of
218
279
324
319
366
383
interventions
20012002
Figure 4 Comparison of interventions by pharmacists.
Number of interventions
20002001
Number of interventions
20012002
