and by interviewing project leaders at other hospitals to learn
how to apply their successes to our institution. Through this
communication with end-users of information, we were able to
determine the degree of effectiveness at our own institution.
We addressed the challenge of improving our patient care
and pharmacy services primarily from the federal Agency for
Healthcare Research and Quality (AHRQ) model. This agency
had developed a process of evaluating pharmaceutical out-
comes to assess the outcomes projects that it was funding. We
found this methodical tool simple enough to execute and de-
velop within the limitations of our resources, and we used it
successfully to evaluate our progress. Each "challenge" was
presented with a "plan of approach," a "data source," and an
evaluation of the "outcomes and impact of intervention." Our
goal was to seek new knowledge about clinical outcomes to in-
fluence our pharmacy practice guidelines and drug therapy pol-
icy. We believed that measuring the cost-effectiveness of phar-
maceutical interventions and evaluating changes in patient
therapies was the best way to ensure the success of our pro-
gram. Over time, we created our own model of expertise
through the routine exercise of communicating within our
multidisciplinary health care team, which then allowed every-
one involved to comprehend what we were trying to accom-
plish and how we were going to achieve it.
All of our energies focused on clinical pharmacy interven-
tions for ambiguous orders, incorrect dosing, drug interac-
tions, intravenous-to-oral conversions, and adjustments to renal
dosing. Through this practice, we continuously built upon our
efforts by identifying important factors relating to pharmacy
and patient care. Unexpected findings during the course of the
program helped us to expand our goals. Using the AHRQ
model's performance measurement table, we evaluated our
success by presenting challenges in the form of what we hoped
to accomplish. We then established an approach and simply ex-
plained how we would accomplish it.
After we executed our planned approach and gathered our
data, we evaluated the impact of our intervention to assess our
accomplishments. After evaluating the challenge, we reflected
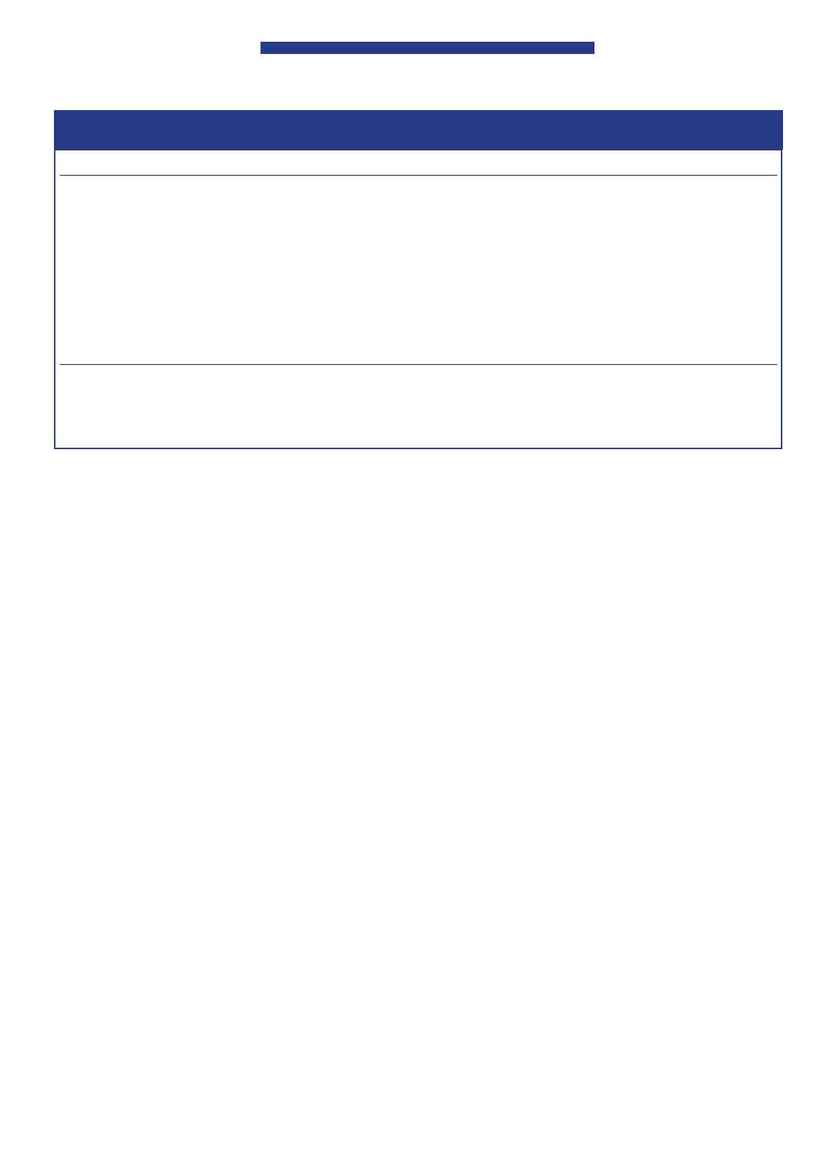
Unit-Specific Pharmacists
54 P&T
®
· January 2003 · Vol. 28 No. 1
IV Medication
Oral Medication
Renal Dosing CrCl < 40
Famotidine (Pepcid®, Merck) 20 mg q12h
Nizatidine (Axid®, Reliant) 150 mg q12h
Nizatidine 150 mg q24h
Fluconazole (Diflucan®, Pfizer) 400 mg q24h
Fluconazole 200 mg q24h
Fluconazole 200 mg q24h
Fluconazole 100 mg q24h
Gatifloxacin (Tequin®, Bristol-Myers Squibb)
Gatifloxacin 400 mg q24h
Gatifloxacin 200 mg q24h
400 mg q24h
Gatifloxacin 200 mg q24h
Gatifloxacin 200 mg q24h
Ciprofloxacin (Cipro®, Bayer) 400 mg q12h
Ciprofloxacin 500 mg q12h
Consult physician for
dose adjustment
Ciprofloxacin 200 mg q12h
Ciprofloxacin 250 mg q12h
Consult physician for
dose adjustment
Pantoprazole (Protonix®, Wyeth-Ayerst) 40 mg q24h Pantoprazole 40 mg q24h
Criteria necessary for automatic IV to PO conversion:
· Patient is taking other medications orally
· Patient has a functional gut and is eating
· Patient has been receiving the IV form for at least 48 hours
CrCl = creatinine clearance; IV = intravenous; PO = oral.
Table 1 Medications Approved for Automatic Intravenous-to-Oral Conversion
on the entire process to determine whether we could apply the
findings to other areas. Table 2 presents our actual perfor-
mance measurement.
Our collected data included the number of missing medi-
cations, dosing adjustments, intravenous-to-oral drug conver-
sions, and adverse drug reactions. The information was doc-
umented and obtained primarily via direct observation by
clinical pharmacists on a daily basis.
Our program's success has prompted the hospital's admin-
istrators to expand the clinical pharmacy program from three
nursing units to all patient-care areas with patient stays longer
than 24 hours, with a proposal to extend this period to seven
days a week. We obtain patient laboratory data directly from
our laboratory department through electronic resources in
the institution or from the patient's chart. We record the data
pertaining to all of our interventions on Microsoft Excel
®
spreadsheets once a month to present to the P&T committee,
and we confirm the accuracy and completeness of our data
when the clinical pharmacists consult with colleagues on the
multidisciplinary team. Despite the small size of our hospital,
we have developed the ability to communicate effectively with
the entire multidisciplinary team on a daily basis.
After the program became part of the daily pharmacist ros-
ter assignment and the pharmacists became familiar with the
routine, we reported our first experiences to other committees
that were also concerned with preventing medication errors.
Although the data were uniform and consistent, the emphasis
varied, depending on the focus of the committee. We notified
the administration of any problems or changes in the pro-
gram's progress.
Our report to the P&T committee during the first couple
of months of the program demonstrated a three-fold increase
in the number of interventions documented (Figure 4). This
result was considered to have a positive effect on improving
patient care, in documenting potential errors and near-misses,
and in conserving hospital resources.
The data that we have been collecting are ongoing and dy-
namic, and they clearly show changes in patient care simply
